© Academy for innovation in medical sciences
GIRL CURED WITH PHAGE THERAPY
AFTER 4 YEARS OF INEFFECTIVE ANTIBIOTIC TREATMENTS
Alice, a 25-year-old girl born in Treviso and living in the province of Venice. An ordeal that now seems to be over, and a hope that is rekindled. She underwent treatment under the care of Dr. Alfonso Recordare at the Ospedale Dell'Angelo in Mestre.
Chronic post-traumatic osteomyelitis of the tibia resolved with phage therapy.
Case description
Alfonso Recordare, Nikoloz Pruidze*, Lia Nadareishvili*, Dea Nizharadze*. MziaKutateladze*
Div. Surgery Ospedale dell'Angelo Venice Mestre, Italy. *EliavaPhageTherapyCenter Tbilisi, Georgia
A CLINICAL CASE IN ITALY - 1
Osteomyelitis is one of the most serious infectious complications in patients undergoing fracture reduction with fixation devices.
The standard treatment for the most advanced stages involves a combination of surgical therapy and antibiotics.
These infections often do not resolve due to the emergence of antibiotic resistance, poor ability to penetrate the biofilm, or other factors. Bacteriophages represent a valid aid in the treatment of these complex forms.
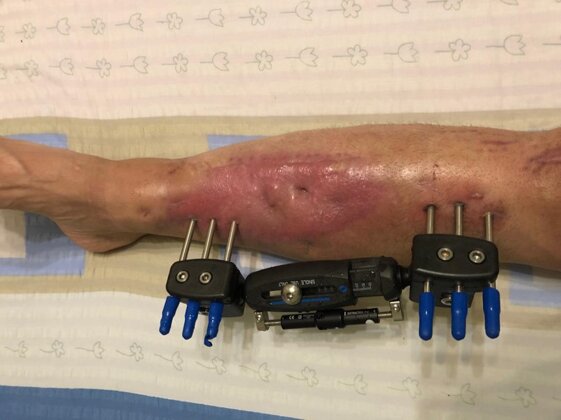
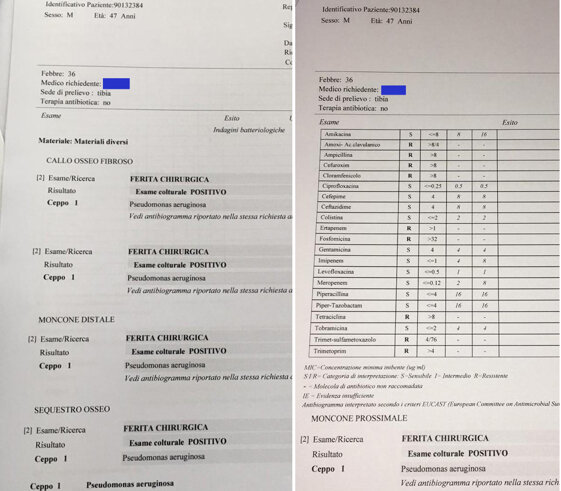
PHOTO - 1
Clinical picture at the beginning of treatment with bacteriophages. The patient presents with spontaneous pain and is able to walk with the aid of crutches for short distances.
There is an actively secreting fistula and signs of inflammation in the middle and lower third of the leg.
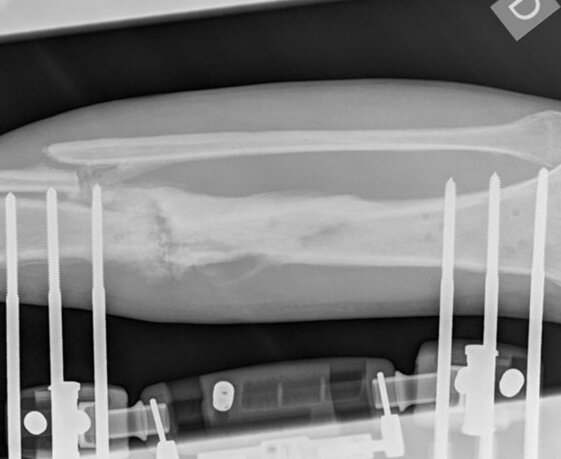
PHOTO - 2
Radiological check-up one month after the start of therapy. The fistula has closed.
The X-ray examination shows the formation of bone callus, mainly on the side opposite to the insertion of the external fixators, and signs of consolidation of the pseudoarthrosis site.

PHOTO - 3
Clinical picture 40 days after the start of treatment. A fistula appears, secreting a modest amount of serum.
A culture test reveals a staphylococcus, sensitive to a different preparation of bacteriophages (staphylophage®), which is added to the ongoing therapy.

PHOTO - 4
Clinical picture at the end of therapy. The fixation devices have been removed. After a period of 30 days in a plaster cast, the patient walks without the need for any aid. At the 3-month follow-up, the skin condition is progressively improving and the bone callus is undergoing progressive ossification.
At 2 years, there are no signs of recurrence, either clinical or biochemical.